Asthma Self Care: Essential Tips to Control Symptoms
Living with asthma can feel unpredictable, which is why strong asthma self care habits matter more than most people realize. Whether you manage symptoms daily or only face occasional flare-ups, understanding asthma self care is one of the most effective ways to stay in control and breathe with confidence. Many people rely solely on medication, but small daily choices, like avoiding triggers or improving your home environment, can dramatically reduce symptoms and prevent unnecessary stress.
This topic matters because asthma is not just a medical condition, it’s part of your lifestyle. Knowing how to respond to early warning signs, follow an asthma action plan, or support your lungs through healthy routines can help you stay ahead of flare-ups instead of reacting to them. With the right approach, asthma self care becomes a realistic, empowering system rather than a complicated task.
In this guide, you’ll find practical steps, expert-backed strategies, and simple habits that make managing asthma easier every day. Let’s start by breaking down what really works and why it can make such a difference.
Chapter 2: Understanding Asthma and Why Self Care Matters
Asthma affects more than 300 million people worldwide, yet many people still struggle to understand how the condition actually works and why consistent asthma self care matters so much. If you or someone in your family lives with asthma, you already know how unpredictable symptoms can be. One week may feel completely normal, and the next can bring tightness, wheezing, or sudden flare-ups that interrupt sleep, work, and daily routines. This unpredictability is exactly why self care is not just helpful, but essential. Effective asthma self care keeps inflammation low, stabilizes breathing, and reduces the risk of emergency episodes.
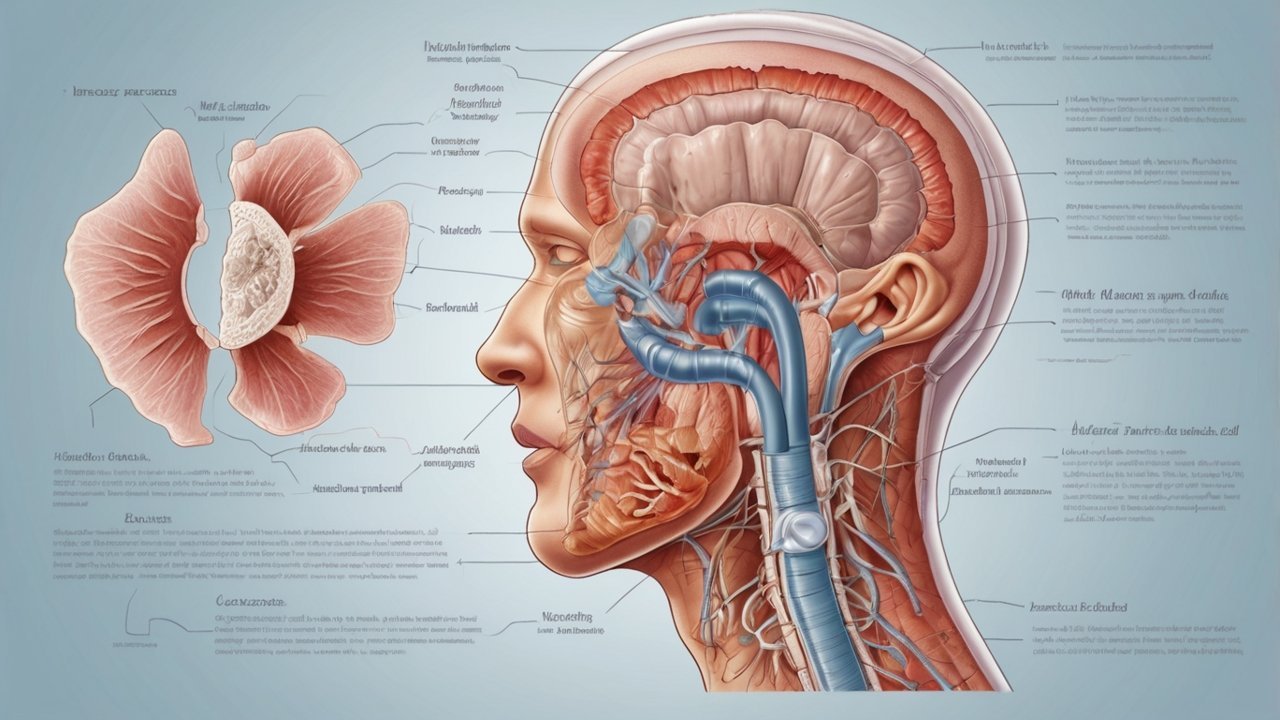
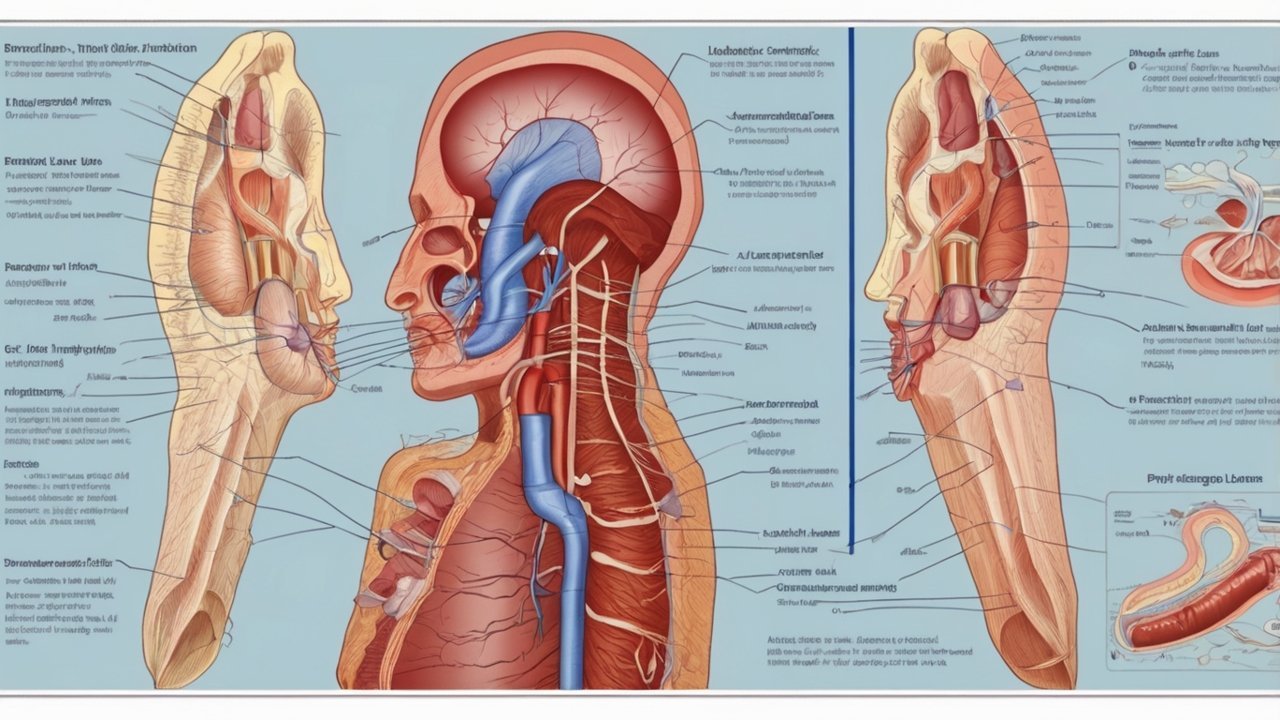
What’s Really Happening Inside Your Airways
Asthma is a chronic inflammatory disease. When exposed to triggers like pollen, dust, smoke, cold air, or stress, the airway lining swells and the surrounding muscles tighten. This narrows the bronchial tubes and makes breathing feel strained. Harvard Health notes that inflammation often persists quietly in asthma patients even between flare-ups, which is why proactive care can dramatically lower risk and improve stability (Harvard Health Publishing, 2023).
A 2022 PubMed review also highlights that long-term inflammation management is more effective than occasional symptom relief, reinforcing the importance of everyday habits rather than reactive treatment (PubMed, 2022).
Why Self Care Matters More Than Most People Realize
Medication alone is not enough. The most stable asthma patients are usually those who combine medication with a structured routine of understanding triggers, tracking symptoms, and improving their environment. Think of an asthma inhaler as a seatbelt. It protects you in emergencies, but the way you drive every day reduces your overall risk.
Consistent asthma self care helps you:
• Reduce flare-ups
• Improve lung function
• Feel more confident in daily life
• Reduce healthcare costs
• Stay active with fewer limitations
If you’re working on improving overall wellness as part of your self-care journey, you may find energy-supporting content helpful, such as:
Mitochondrial Energy Boost
The Role of Triggers in Long-Term Control
Most asthma flare-ups are triggered by environmental or lifestyle factors. Common triggers include:
• Dust mites
• Mold
• Pet dander
• Strong fragrances
• Cold or dry air
• Viral illnesses
• Stress and anxiety
• Seasonal allergies or pollen
A Journal of Asthma study found that reducing indoor allergens could cut flare-ups by nearly 50 percent for many patients. This shows that self care is not just about inhalers, but about daily choices and home management.
For seasonal trigger management tips, you may find this guide useful:
Seasonal Wellness Natural Tips
A Practical Example: Two Patients, Two Outcomes
Patient A (Reactive Approach)
• Uses inhaler only when symptoms appear
• Doesn’t track triggers
• Sleeps poorly due to uncontrolled symptoms
Patient B (Proactive, Self Care Approach)
• Tracks symptoms
• Avoids known triggers
• Follows a clear asthma action plan
• Uses controller medication consistently
Patient B experiences fewer flare-ups, more predictable breathing, and more stable energy levels. The difference isn’t luck. It’s habit.
Lifestyle Habits That Improve Asthma Stability
You don’t need huge changes. Small, consistent improvements matter most:
• Wash bedding weekly
• Use HEPA filtration
• Keep humidity between 40–50%
• Choose fragrance-free cleaners
• Get enough sleep
• Practice gentle breathing exercises
• Stay hydrated
• Eat anti-inflammatory foods
If you’re exploring nutrition to support overall wellness, you can also check:
Top Superfoods to Boost Energy →
Tools and Resources That Make Self Care Easier
Some people prefer structured tools to help them stay consistent.
Daily Habit Tracking Tool
If you want a simple way to track symptoms, triggers, breathing quality, and routines, this guide recommends a helpful tracker:
Check this recommended tool here →
Lifestyle Support Supplements
Some individuals prefer additional lifestyle support for inflammation and wellness. If you’re exploring options, you can review this affordable supplement solution:
Discover this affordable solution today →
These tools are optional and meant to complement medical care, not replace it.
Pros and Cons of Asthma Self Care Strategies
| Strategy | Pros | Cons |
|---|---|---|
| Medication only | Quick relief | Doesn’t prevent flare-ups |
| Medication + minimal habits | Helps with daily control | Still exposed to triggers |
| Full asthma self care plan | Best long-term control, fewer emergencies | Requires consistency |
The Takeaway: Your Daily Choices Shape Your Breathing
Asthma is not a once-in-a-while condition. It’s a daily interaction between your lungs and your environment. When you understand what’s happening in your airways and how your habits influence inflammation, you reclaim control. Effective asthma self care is not complicated, but it does require intention. The more consistent your habits, the easier breathing becomes over time.
Chapter 2: Build Your Personal Asthma Action Plan
Every person with asthma needs a clear action plan. It is the roadmap you follow when symptoms shift, triggers appear, or flare-ups begin to build. A strong plan is one of the most reliable foundations of asthma self care, because it removes guesswork and helps you respond early rather than reacting late. Whether you’ve had asthma for years or were diagnosed recently, an action plan gives you confidence, structure, and a predictable way to protect your breathing.
Why an Asthma Action Plan Matters
Asthma symptoms can change quickly. What feels like mild tightness at noon can turn into a significant flare by evening if you ignore early warning signs. The American Lung Association and multiple PubMed studies highlight that patients with a written action plan have better symptom control, fewer hospital visits, and more stable lung function.
An asthma plan helps you:
• Recognize early symptoms
• Know exactly which medication to use and when
• Track triggers more accurately
• Prevent flare-ups instead of reacting to them
• Stay calm during breathing changes
• Improve communication with doctors and family
If Chapter 1 explained the “why” behind asthma self care, this chapter explains the “how.”
Step 1 — Track Your Symptoms Consistently
A plan begins with awareness. You cannot manage what you do not measure. Tracking symptoms daily helps you see trends you would otherwise miss.
Track things like:
• Morning and evening breathing quality
• Use of rescue inhaler
• Exposure to common triggers
• Physical activity levels
• Sleep quality
• Stress levels
• Any unusual environmental changes
Many patients prefer to use digital trackers, journals, or simple daily templates. If you want a beginner-friendly system that helps you record symptoms and lifestyle habits in one place, consider this helpful tool:
Check this recommended tool here →
It simplifies long-term monitoring, which strengthens your asthma self care routine.
Step 2 — Understand Your Warning Zones (Green, Yellow, Red)
Most asthma action plans use a three-zone approach:
Green Zone (Stable Breathing)
You feel well, breathe normally, and use your rescue inhaler rarely. This is where consistent habits matter most: hydration, sleep, clean air, trigger avoidance, and regular controller medication.
Yellow Zone (Symptoms Begin to Appear)
You may notice:
• Mild chest tightness
• Slight wheezing
• Coughing
• Reduced exercise tolerance
• Slight shortness of breath
This is the moment when self care makes the biggest difference. Adjusting medications, reducing triggers, and resting can prevent a flare from escalating.
Red Zone (Flare-Up or Distress)
Breathing becomes difficult, speaking may feel harder, and rescue medication is required quickly. Red zone symptoms mean immediate action — and if symptoms do not improve, seek medical help urgently.
An effective plan tells you exactly which step to take in each zone.
Step 3 — Coordinate Your Plan With Your Doctor
No action plan is complete until you review it with a healthcare provider. They will help you decide:
• Which inhalers to use in each zone
• How often to use controller medication
• When to adjust dosages
• Which symptoms count as emergencies
• Whether allergy testing or immunotherapy might help
• Which lifestyle habits support long-term stability
If you’re curious about how inflammation, metabolism, and immunity interact, these wellness articles can offer additional context:
Mitochondrial Imbalance: The Hidden Cause of Fatigue
Top Superfoods to Boost Energy →
Step 4 — Build a Trigger-Avoidance Checklist
Once you know your personal triggers, create a simple list you can follow at home:
• Wash bedding weekly in hot water
• Use HEPA air filtration
• Keep humidity between 40–50%
• Avoid fragrance-heavy cleaners
• Limit exposure to cold or dry outdoor air
• Manage stress and sleep
• Keep pets out of the bedroom
• Reduce dust buildup with weekly vacuuming
If you want broader seasonal guidance, explore:
Seasonal Wellness Tips
A trigger checklist is easy to update and becomes part of your everyday asthma self care routine.
Step 5 — Prepare an Emergency Plan
An emergency plan ensures you’re never caught off guard.
Include:
• Who to call
• Which medication to take
• When to go to urgent care
• Your doctor’s contact info
• A printed copy for home, work, school, and travel
Sharing the plan with family members, coworkers, or your child’s teachers ensures everyone knows what to do in a crisis.
Step 6 — Support Your Body With Lifestyle Choices
Asthma management is more than medication. Your lungs respond to how you live:
• Hydration supports mucus clearance
• Sleep reduces inflammation
• Gentle exercise strengthens breathing muscles
• A balanced diet helps regulate immune response
If you’re exploring supportive supplements that some people use to enhance overall wellness, you can look into this option:
Discover this affordable solution today →
This is not a replacement for asthma treatment, but many readers find it useful for general health support.
The Takeaway: Your Action Plan Is Your Daily Anchor
Asthma becomes far more manageable when you follow a structured plan. By tracking symptoms, understanding your warning zones, and coordinating care with your doctor, you build a system that protects your breathing and reduces the stress of unpredictability. A smart action plan is not complicated — it’s practical, personalized, and central to effective asthma self care.

Chapter 3: Identify and Control Your Triggers
One of the most important parts of long-term asthma self care is learning to identify and control your personal triggers. Even the best medication routine can fall apart if your environment constantly irritates your airways. Triggers look different for everyone, which is why understanding your unique pattern is essential. Some people react most to seasonal allergies, while others are sensitive to dust, pets, weather changes, or even stress. Once you know what affects you, flare-ups become far more predictable and manageable.
Why Trigger Awareness Matters
Most asthma flare-ups are not random. In fact, studies from the National Heart, Lung, and Blood Institute show that the majority of asthma episodes begin with exposure to something that irritates inflamed airways. This could be pollen floating in through a window, or something as subtle as a change in humidity.
Understanding your triggers helps you:
• Prevent symptoms before they start
• Reduce nighttime coughing
• Stay active with fewer restrictions
• Keep medication use predictable
• Protect your lungs long-term
Trigger awareness connects directly with effective asthma self care, because avoiding irritants gives your lungs the break they need to stay calm.
Common Asthma Triggers and How to Reduce Exposure
While everyone’s list is unique, certain triggers affect most people with asthma. Below are the most common ones, plus simple ways to reduce exposure.
1. Dust Mites and Indoor Allergens
Dust mites thrive in bedding, upholstery, carpets, and curtains. They are one of the most common asthma triggers, especially for people living in humid climates.
How to reduce dust exposure:
• Wash bedding weekly in hot water
• Use allergen-proof pillow and mattress covers
• Vacuum with a HEPA-filter vacuum (weekly)
• Keep humidity at 40–50%
• Avoid heavy fabric curtains or rugs
If you want broader guidance on creating a cleaner home environment, this seasonal guide can help:
Seasonal Wellness Natural Tips →
2. Mold and Damp Areas
Bathrooms, basements, and kitchens are common mold hotspots. Even small amounts can irritate sensitive airways.
What you can do:
• Use a dehumidifier in damp rooms
• Clean mold-prone areas weekly
• Avoid leaving wet clothes indoors
• Ensure good ventilation
A cleaner home environment directly supports your overall asthma self care routine.
3. Pets and Dander
Pets bring warmth and comfort, but their dander can irritate your airways.
Ways to reduce pet-related triggers:
• Keep pets off the bed
• Use an air purifier
• Brush pets outdoors
• Wash hands after touching them
You don’t have to give up your pets; you only need a good routine.
4. Pollen and Outdoor Allergens
Seasonal allergies and asthma often go hand in hand. Research indicates that pollen exposure significantly increases flare-ups in spring and fall.
To reduce pollen exposure:
• Track pollen counts daily
• Keep windows closed during high-pollen days
• Shower or wash your face after returning home
• Use a HEPA air purifier indoors
For boosting your overall resilience during seasonal changes, this resource may help:
Top Superfoods to Boost Energy →
5. Cold Air and Weather Shifts
Cold or dry air can tighten the airways. Many people feel asthma symptoms worsen during winter or abrupt weather changes.
Helpful habits:
• Wear a scarf over your mouth outdoors
• Warm up before exercise
• Use a humidifier indoors
6. Smoke, Fragrances, and Air Pollution
Strong odors and airborne chemicals can irritate inflamed airways instantly.
Avoid exposure to:
• Cigarette smoke
• Wood-burning stoves
• Scented candles
• Perfumed cleaning sprays
• Smog and pollution
Whenever possible, choose fragrance-free or natural cleaning options.
7. Stress and Emotional Triggers
Stress doesn’t always show up physically, but it affects the nervous system and breathing patterns. Harvard Health reports that emotional stress can worsen asthma in many patients.
Ways to manage stress:
• Deep breathing exercises
• Gentle yoga
• Restful sleep
• A consistent daily routine
For additional self-care support, some people use simple tracking tools. If you want a structured way to track stress, sleep, and symptoms together, consider this option:
Check this recommended tool here →
How to Identify Your Personal Triggers
Not all triggers are obvious. Some build slowly, like humidity changes. Others are fast and intense, like perfume or cigarette smoke.
Here’s how to discover your own:
1. Keep a symptom diary
Record when symptoms happen, what you were doing, and where you were.
2. Track patterns across weeks
Do symptoms worsen in the morning? After cleaning? After being outdoors?
3. Use smartphone apps or digital trackers
These help spot patterns you may not notice.
4. Consider allergy testing
Your doctor can help identify allergic triggers through skin or blood tests.
5. Adjust one variable at a time
This makes it easier to identify the true cause.
Extra Supportive Options (Optional Enhancements)
Some people like pairing lifestyle habits with wellness support, especially during allergy-heavy seasons. If you’re exploring such options, you can review this affordable supplement:
Discover this affordable solution today →
This is not a medical treatment for asthma, but it may support general wellness.
The Takeaway: Control Your Environment, Control Your Breathing
Identifying and avoiding triggers is one of the most reliable forms of asthma self care. When you understand what irritates your airways, you protect your lungs from inflammation before symptoms begin. You’ll breathe easier, experience fewer flare-ups, and feel far more confident in daily life. Small changes add up, and your lungs will thank you for it.
Chapter 4: Daily Asthma Self Care Habits
Daily habits shape how well your lungs function, how often symptoms appear, and how predictable your breathing feels. While medication plays a central role in asthma management, the most stable patients are usually the ones who combine medical treatment with consistent lifestyle habits. These small daily routines are the backbone of effective asthma self care and can dramatically reduce flare-ups over time.
Asthma doesn’t have to control your schedule or limit your possibilities. When you support your lungs through meaningful routines, you create an environment where your airways stay calmer, more resilient, and less reactive to triggers.
Why Daily Habits Matter for Asthma Stability
Asthma is a chronic inflammatory condition, and inflammation doesn’t take days off. That means your habits shouldn’t either. The goal of asthma self care is to reduce everyday irritation so your medications can work more effectively.
According to a review published in Chest Journal, patients who maintain consistent routines such as inhaler adherence, sleep hygiene, and exercise experience fewer hospital visits and higher quality of life (PubMed, 2022). Daily habits are not just helpful. They’re essential.
Proper Inhaler Technique (Often Overlooked)
Most people think they’re using their inhaler correctly, but research from Harvard Health shows that up to 70 percent of asthma patients use improper technique, reducing medication effectiveness.
Checklist for correct inhaler use:
• Shake the inhaler
• Exhale fully before inhaling
• Seal lips tightly around the mouthpiece
• Press the inhaler and inhale slowly
• Hold breath for 5–10 seconds
• Exhale gently
If your doctor recommended using a spacer, it can significantly improve medication delivery to the lungs.
Spacer tips:
• Ensure proper seal
• Clean weekly with mild soap
• Let it air dry to avoid static
These small adjustments can drastically improve medication efficiency and are a key part of good asthma self care.
Breathing Exercises to Improve Lung Function
Breathing exercises help strengthen respiratory muscles, calm the nervous system, and improve airflow.
Three exercises shown to help asthma patients:
1. Diaphragmatic Breathing
• Sit upright
• Place one hand on your belly
• Inhale through your nose, pushing your stomach out
• Exhale fully through your mouth
2. Pursed-Lip Breathing
Helps keep airways open longer.
• Inhale for 2 seconds
• Exhale slowly through pursed lips for 4–6 seconds
3. Box Breathing
Useful during stress-triggered asthma episodes.
• Inhale 4 seconds
• Hold 4 seconds
• Exhale 4 seconds
• Hold 4 seconds
For improving sleep and relaxation, this article can help:
Yoga Nidra for Sleep →
Build a Lung-Friendly Home Environment
Your home environment directly affects your breathing. Even if your lungs feel stable, hidden triggers—dust, mold, pet dander—can quietly increase inflammation.
Simple improvements that make a big difference:
• Use a HEPA air purifier
• Vacuum weekly with HEPA filtration
• Wash bedding weekly
• Keep humidity around 40–50%
• Ventilate rooms daily
• Avoid harsh chemical cleaners
• Reduce clutter where dust collects
For seasonal adjustments, check this helpful guide:
Seasonal Wellness Tips →
Exercise and Movement: Yes, You Can Be Active
Exercise is not the enemy of asthma — uncontrolled asthma is.
Physical activity improves lung strength, reduces inflammation, and enhances overall stamina. Many asthma patients find that regular, moderate-intensity movement leads to fewer symptoms over time.
Best exercises for asthma:
• Walking
• Yoga
• Swimming
• Cycling
• Light jogging
• Low-impact strength training
If you’re building a home fitness routine, this guide offers beginner-friendly ideas:
Home Workout Plan for Beginners →
Exercise tips for asthma patients:
• Warm up slowly
• Avoid exercise in cold, dry air
• Keep your rescue inhaler nearby
• Cool down for 5–10 minutes afterward
Nutrition and Hydration for Better Breathing
Food may not cure asthma, but it can support your body’s inflammatory and immune responses.
Lung-friendly foods include:
• Leafy greens
• Sweet potatoes
• Berries
• Fatty fish
• Olive oil
• Citrus fruits
You can explore more nutrition insights here:
Top Superfoods to Boost Energy →
Hydration also helps keep mucus thin and easier to clear.
Stress Management as a Form of Asthma Care
Stress is a trigger for many asthma patients. Emotional tension can tighten the chest, affect breathing rhythm, and increase airway inflammation.
Ways to manage stress daily:
• Guided meditation
• Gentle yoga
• Deep breathing
• Restful sleep
• Time outdoors
• A consistent routine
To support habit-building and stress tracking, this digital tool may help:
Check this recommended tool here →
Optional Lifestyle Enhancements
Some readers explore wellness supplements to support energy, gut health, and inflammation, especially during high-trigger seasons.
If you’re interested in options, you can review this affordable solution:
Discover this affordable solution today →
(Not a replacement for asthma medication.)
Final Thoughts: Small Habits, Big Changes
Daily habits are the heart of strong asthma self care. They give you more predictable breathing, fewer disruptions, and more freedom to live life the way you want. By supporting your lungs through movement, environment, nutrition, and mindfulness, you create a lifestyle that keeps your airways calmer and more resilient.
Asthma may be a long-term condition, but it does not need to control your day-to-day life. Your habits shape your health — one choice at a time.

Chapter 5: Home Environment Tips for Better Breathing
Your home should be the place where your lungs feel safest. But for many people with asthma, the indoor environment contains more triggers than the outdoors. Dust mites, mold, chemical cleaners, stale air, and pet dander can quietly irritate the airways every day. Improving your home environment is one of the most powerful forms of asthma self care, because you spend most of your time indoors — especially during sleep, when breathing patterns are most vulnerable.
The good news is that even small changes can dramatically reduce inflammation and help stabilize your breathing. You don’t need a complete home makeover. You need smart, consistent adjustments that protect your airways from common irritants.
Why Your Indoor Environment Matters
Studies from the Environmental Protection Agency (EPA) show that indoor air can be two to five times more polluted than outdoor air. For someone with asthma, this means the home environment can significantly impact flare-ups, nighttime coughing, and overall lung comfort.
A review published in The Journal of Asthma found that improving indoor air quality led to fewer symptoms and fewer emergency visits, especially in people sensitive to dust and mold (PubMed, 2021). So, improving your environment isn’t optional — it’s central to sustainable asthma self care.
Air Purifiers: Do They Really Help?
Yes — but only if you choose the right type. A true HEPA filter captures small particles like dust mites, pollen, smoke, and pet dander.
Benefits of HEPA air purifiers:
• Reduced airborne allergens
• Better sleep quality
• Lower dust accumulation
• Cleaner airflow during pollen season
Where to place them:
• Bedroom (most important)
• Living room
• Home office or kitchen
If you’re looking to support your broader wellness goals alongside cleaner air, check out:
Seasonal Wellness Tips →
Humidity Control: The Silent Game-Changer
Humidity between 40–50% is ideal for asthma patients. Lower humidity dries out the airways, making them more reactive. High humidity encourages mold and dust mites.
Tools that help:
• A humidifier for dry climates
• A dehumidifier for damp climates
• A humidity monitor (very inexpensive and effective)
Humidity management is one of the easiest and most underrated forms of asthma self care.
Cleaning Routines That Protect Your Lungs
Asthma-friendly cleaning doesn’t mean constant scrubbing. It means smart timing and the right tools.
Weekly routine:
• Vacuum carpets and rugs with a HEPA vacuum
• Wipe hard surfaces with fragrance-free sprays
• Wash bedding in hot water
• Clean bathroom tiles to prevent mold
• Declutter areas where dust collects
Fragrance-free cleaners are essential. Strong scents can trigger immediate airway irritation. If you want guidance on safe household products and a clean-living lifestyle, explore:
Low-Sodium Diet & Healthy Choices →
(Not directly asthma-related, but useful for overall health-conscious living.)
Pets and Asthma: Finding the Balance
You don’t need to give up your pets. You simply need pet-friendly routines.
Tips to reduce dander exposure:
• Keep pets out of the bedroom
• Use an air purifier
• Groom pets outdoors when possible
• Wash pet bedding weekly
• Choose hard surfaces over carpets when possible
These basic habits can reduce flare-ups significantly.
Bedroom Upgrades for Asthma Relief
Your bedroom is the most important area to optimize, because nighttime asthma symptoms often go unnoticed.
Bedroom improvements:
• Allergen-proof mattress and pillow covers
• Minimal decor to reduce dust
• Wash sheets weekly
• Replace old pillows every 1–2 years
• Avoid scented candles or diffusers
• Keep windows closed during high-pollen days
Many readers pair home upgrades with wellness tracking. If you want to monitor sleep quality, stress, and breathing patterns, consider this simple tool:
Check this recommended tool here →
Kitchen and Cooking Habits
Strong cooking fumes can irritate airways, especially if your home has poor ventilation.
Helpful kitchen habits:
• Use the exhaust fan while cooking
• Avoid high-smoke oils
• Keep windows slightly open if weather allows
• Clean oil buildup around stoves
Mold Prevention Checklist
Mold thrives in damp, dark spaces.
Prevent mold by:
• Fixing water leaks quickly
• Using ventilation in bathrooms
• Cleaning shower curtains and tiles
• Drying wet laundry promptly
• Running a dehumidifier in damp rooms
This checklist is essential for long-term asthma self care.
Optional Wellness Enhancements
Some readers prefer additional support during allergy-heavy seasons or stressful months. If you’re exploring lifestyle-support supplements, you can review this option:
Discover this affordable solution today →
(Not a replacement for asthma medication.)
Final Thoughts: Your Home Should Help You Breathe Easier
You don’t need a perfect home — you need a mindful one. By adjusting humidity, improving airflow, cleaning smarter, and reducing allergens, you create a living space that supports stable breathing year-round. These simple habits are not just about comfort. They’re foundational to effective asthma self care, helping you reduce flare-ups, sleep better, and protect your lungs every day.

Chapter 6: Lifestyle Strategies to Strengthen Lung Health
Asthma management is not only about medication, doctor visits, or emergency preparedness. The way you live day to day has a powerful impact on your lungs. Small lifestyle choices influence inflammation, airway sensitivity, breathing patterns, and overall resilience. Many asthma patients underestimate how profoundly sleep, nutrition, hydration, physical activity, and stress shape their symptoms. Strengthening your lung health through intentional habits is a core part of effective asthma self care, and it can dramatically improve your long-term stability.
You don’t need to overhaul your entire lifestyle. Instead, focus on building steady habits that support your breathing from the inside out.
Exercise: Why Movement Helps Your Lungs Work Better
Exercise might feel intimidating for some asthma patients, especially if exertion has triggered symptoms in the past. But when practiced safely, movement is one of the most powerful tools for improving lung strength.
Research published in Frontiers in Physiology shows that regular training helps improve airway elasticity, oxygen efficiency, and respiratory muscle stamina (PubMed, 2020). In other words, the more consistently you move, the easier breathing becomes.
Best asthma-friendly exercises:
• Walking or brisk walking
• Swimming (warm, humid air is gentler on airways)
• Yoga or Pilates
• Light jogging
• Cycling
• Low-impact strength training
If you want a gentle, at-home workout to get started, this beginner guide is helpful:
Home Workout Plan for Beginners →
Exercise tips for asthma patients:
• Warm up slowly (5–10 minutes)
• Avoid exercising in very cold or dry air
• Keep your rescue inhaler nearby
• Cool down gradually
• Hydrate before and after workouts
Regular movement reduces stress and inflammation, making it a foundational part of asthma self care.
Nutrition: Eating for Lower Inflammation and Better Breathing
Food doesn’t cure asthma, but it directly affects inflammation levels, mucus production, immune function, and energy. A 2021 Harvard Health review found that anti-inflammatory diets rich in fruits, vegetables, healthy fats, and whole foods support lung performance and reduce airway reactivity.
Lung-supportive foods include:
• Sweet potatoes
• Berries
• Leafy greens
• Fatty fish
• Olive oil
• Turmeric and ginger
• Citrus fruits
• Whole grains
If you want guidance on nutrient-rich foods that support immune and energy function, check this article:
Top Superfoods to Boost Energy →
Foods that may worsen asthma symptoms:
• Processed meats
• Sugary drinks
• Artificial additives
• High-sodium packaged foods
• Fried foods
Small nutrition improvements lead to better energy and fewer inflammatory spikes — both essential to consistent asthma self care.
Hydration: Keeping Airways Moist and Functional
Hydration is often overlooked, but it plays a key role in how your lungs function. Dry airways are more reactive, meaning irritants can trigger symptoms faster.
Benefits of staying hydrated:
• Helps thin mucus
• Supports smooth airflow
• Improves exercise performance
• Reduces throat irritation
• Helps calm coughing
Aim for steady hydration throughout the day. Herbal teas, water-rich fruits, and plain water are excellent choices.
Sleep: Your Nighttime Lung Reset
Sleep is when your body repairs tissue, regulates immune activity, and restores hormonal balance. Poor sleep increases inflammation and can make airways more sensitive.
A study published in The Lancet Respiratory Medicine found strong associations between poor sleep quality and increased asthma symptoms.
Better sleep strategies:
• Maintain a regular bedtime
• Keep your bedroom allergen-free
• Avoid late caffeine
• Use a HEPA purifier at night
• Practice a calming pre-sleep routine
For improved sleep quality, many readers find mind-body techniques helpful:
Yoga Nidra for Sleep →
Quality sleep supports every other part of asthma self care by lowering inflammation and helping your body remain resilient.
Stress Management: Protecting Your Airways From Emotional Triggers
Stress is a surprisingly powerful asthma trigger. Emotional tension tightens chest muscles, disrupts breathing patterns, and increases airway inflammation — especially in people whose asthma is sensitive to nervous-system changes.
Effective stress reducers:
• Deep breathing
• Meditation
• Short daily walks
• Gentle stretching
• Journaling
• A consistent daily routine
If you want help tracking stress, sleep, and lifestyle patterns all in one place, you can use this simple tool:
Check this recommended tool here →
Optional Wellness Enhancements
Some readers use additional lifestyle supplements to support energy, metabolism, or immune health — especially during seasons when asthma feels more sensitive. If you’re exploring options, here’s one commonly recommended resource:
Discover this affordable solution today →
(This is NOT a medical treatment and does not replace asthma medication.)
The Takeaway: Healthy Habits Make Breathing Easier
Lifestyle isn’t everything — but it shapes far more of your asthma journey than most people realize. Movement, sleep, nutrition, hydration, and stress management all influence how your lungs respond to triggers. When these habits become part of your daily rhythm, you gain more predictable breathing and fewer interruptions to your life.
Strong asthma self care is built on small, consistent choices. They help your lungs stay calmer, your energy stay higher, and your flare-ups become far less frequent.

Chapter 7: Special Considerations for Children and Older Adults
Asthma doesn’t look the same for everyone. Children and older adults often experience symptoms differently from the average adult, and their care needs can be more nuanced. Understanding these differences is essential for effective asthma self care, especially if you’re a parent, caregiver, or someone supporting an older family member. Their lungs may respond to triggers faster, their symptoms may appear differently, and their treatment routines may require additional structure or monitoring.
This chapter helps you understand how asthma presents in these two age groups, how to spot early warning signs, and how to create environments that support safe, stable breathing every day.
Asthma in Children: Unique Challenges and Solutions
Asthma is one of the most common chronic conditions in childhood. According to the Centers for Disease Control and Prevention (CDC), millions of children experience asthma symptoms each year, often triggered by allergens, infections, or physical activity. Children tend to have smaller airways, which makes them more sensitive to irritation and inflammation.
Common signs of asthma in children
• Frequent coughing (especially at night)
• Wheezing or whistling sounds
• Chest tightness
• Faster breathing
• Trouble keeping up during play
• Fatigue caused by nighttime symptoms
Young children don’t always communicate symptoms clearly, so observing patterns becomes essential.
How Parents Can Support a Child With Asthma
Children thrive with structure, and that includes asthma management. A consistent routine helps them recognize their own symptoms and feel more confident.
1. Create a child-friendly asthma action plan
Break the plan into simple steps and use colors or icons so kids can understand what to do when they feel different levels of symptoms.
2. Teach inhaler technique early
Many flare-ups in children come from incorrect use of inhalers or nebulizers. Pediatricians often recommend using a spacer to help children receive the full dose.
3. Manage the home environment
Kids spend more time indoors, especially during sleep. Improving air quality has a significant impact on reducing flare-ups.
For seasonal adjustments and cleaner-living strategies, you may find this helpful:
Seasonal Wellness Tips →
4. Stay ahead of infection seasons
Colds and viral infections are major triggers in children. Supporting general immune health through nutrition, hydration, and rest helps protect their breathing.
School and Daycare: Safety Measures Every Parent Should Consider
Parents can’t control every environment, but they can help teachers and caregivers prepare.
Provide schools with:
• A copy of the asthma action plan
• A rescue inhaler with clear instructions
• Contact information
• Trigger awareness (e.g., strong perfumes, dust, chalk)
• A note explaining activity limitations if needed
Teach children these simple habits:
• Speak up early when they feel chest tightness
• Avoid heavy running on cold days
• Use their inhaler before strenuous activities if prescribed
Asthma in Older Adults: What Makes It Different?
Asthma in older adults often becomes more complex due to:
• Weaker respiratory muscles
• Reduced lung elasticity
• Co-existing conditions (heart disease, arthritis, diabetes)
• Side effects from multiple medications
• Delayed symptom recognition
Because older adults may not always notice increasing symptoms right away, consistent monitoring becomes a crucial part of their asthma self care.
How to Support Older Adults With Asthma
1. Make medication routines easy and consistent
Older adults benefit from simple, clear routines. Use labeled pillboxes or daily checklists to prevent missed doses.
If you need an easy tool for logging habits, symptoms, or medication patterns, consider:
Check this recommended tool here →
2. Review inhaler technique regularly
Age-related changes — such as arthritis or decreased hand strength — may make some inhalers harder to use. Doctors can recommend alternatives if needed.
3. Keep the living environment safe
Dust, mold, and poor ventilation can affect older adults more strongly than younger individuals. Make sure their home stays clean, well-lit, and well-ventilated.
4. Watch for hidden symptoms
Older adults may mistake asthma symptoms for aging or fatigue.
Watch for:
• Increased coughing
• Shortness of breath during normal activities
• Difficulty sleeping
• Wheezing
5. Support general wellness
Because older adults may have lower energy or chronic inflammation, lifestyle support can be helpful. If exploring gentle wellness support, some readers review this affordable option:
Discover this affordable solution today →
(Not a medical treatment.)
Emotional and Social Factors for Both Groups
Children may feel scared or embarrassed about asthma. Older adults may feel frustrated or overly dependent. Emotional support matters as much as medical routines.
Encourage:
• Open conversations
• Family involvement
• Reassurance during flare-ups
• Gentle empowerment (“You handled that well!”)
Reducing fear can reduce stress — and stress reduction is a proven part of effective asthma self care.
The Takeaway: Asthma Care Should Be Personalized, Not One-Size-Fits-All
Children and older adults experience asthma through different lenses — physically, emotionally, and socially. But both groups benefit deeply from structure, awareness, and supportive environments. By understanding their unique needs, you can help them prevent flare-ups, stay active, and enjoy better quality of life.
At every life stage, strong asthma self care helps build confidence and stability. When you adapt habits, routines, and environments to match these needs, you give your loved ones the best chance at safe, steady breathing.

Chapter 8: When You Should Seek Medical Help
Asthma is manageable for most people, but knowing when to seek medical care is essential. Even with perfect routines and consistent asthma self care, flare-ups can happen when you least expect them. Recognizing early warning signs prevents emergencies and helps you stay safe. Many asthma-related hospital visits occur because people ignore the early stages of breathing difficulty, assuming symptoms will fade on their own. The truth is that delayed treatment often leads to more severe episodes.
In this chapter, we’ll break down the signs that require medical attention, how to act quickly, and why early care is one of the smartest forms of asthma prevention.
Understanding the Difference Between Mild, Moderate, and Severe Symptoms
Not all asthma symptoms are created equal. Some are warning signs. Others signal that your airways are tightening rapidly and need immediate intervention.
Mild symptoms may include:
• Occasional coughing
• Slight chest tightness
• Mild wheezing
• Shortness of breath during heavy exertion
These symptoms usually improve with rescue medication and proper rest.
Moderate symptoms may include:
• Frequent chest tightness
• Noticeable wheezing
• Breathlessness during normal activities
• Waking up at night coughing
• Needing your inhaler more often
Moderate symptoms are a sign your current routine or medication plan needs adjustment.
Severe symptoms require urgent care:
• Rapid breathing
• Difficulty speaking
• Chest pulling inward with each breath
• Bluish lips or fingernails
• Using rescue inhaler with little or no improvement
• Symptoms worsening within minutes
Severe symptoms indicate airway narrowing and inflammation are increasing dangerously fast.
When Your Asthma Action Plan Says “Call Your Doctor”
Your asthma action plan (created in Chapter 2) plays a major role here. Most plans use the traffic light system: green, yellow, and red zones.
You should contact your doctor when:
• You frequently enter the yellow zone
• Your symptoms worsen despite medication
• You need your rescue inhaler more than twice a week
• You struggle to exercise or take normal walks
• Nighttime symptoms become more frequent
• You wake up short of breath
These patterns show your asthma is not under ideal control. Adjusting treatment early prevents serious flare-ups.
If you need help building a stronger routine, this habit-monitoring tool can support your tracking:
Check this recommended tool here →
Signs You Need Immediate Emergency Care
Asthma attacks progress quickly. If symptoms move from mild to severe within minutes, it’s time for urgent care.
Call emergency services immediately if you experience:
• Struggling to breathe or speak
• Chest tightening severely
• No relief after using a rescue inhaler
• Persistent blue tint on lips or nails
• Confusion or extreme fatigue
• Severe wheezing that grows quieter (a dangerous sign)
During severe attacks, oxygen intake drops — sometimes without the person realizing how bad things have become. Research from The Lancet Respiratory Medicine highlights that early emergency intervention reduces hospital time and speeds recovery.
When Children Need Emergency Care
Children may show asthma distress differently than adults. Watch closely for:
• Belly breathing or ribs pulling in
• Rapid breathing
• Persistent coughing
• Trouble eating or talking
• Lethargy or unusual quietness
• No improvement after medication
Children deteriorate faster because their airways are smaller. When in doubt, act early.
For more guidance on children’s unique asthma needs, visit Chapter 7 or explore helpful wellness support here:
Seasonal Wellness Tips →
When Older Adults Need Medical Help
Older adults may ignore symptoms or assume they’re caused by age or fatigue. But subtle breathing changes are often early signs of flare-ups.
Seek medical help for older adults if they show:
• Increased coughing
• Confusion
• Trouble walking short distances
• Wheezing at rest
• Sleep disturbances
• Dizziness or chest discomfort
Because older adults often take multiple medications, their asthma may require more frequent medical review.
Why Early Intervention Protects Your Lungs
Early medical care prevents small issues from becoming dangerous ones.
Benefits of seeking help early:
• Faster recovery
• Lower chance of hospitalization
• Less airway inflammation
• Reduced long-term lung damage
• More accurate treatment adjustments
Harvard Health emphasizes that delays in treatment are one of the top risk factors for severe asthma outcomes.
Supporting Your Body Before and After a Medical Visit
Even if you need medical care, lifestyle support still matters.
Before a flare-up:
• Notice early signs
• Reduce triggers
• Use your action plan
• Increase hydration
After a flare-up or appointment:
• Follow doctor instructions
• Clean and ventilate your environment
• Track symptoms daily
• Get adequate rest
• Avoid strenuous exercise for several days
To help with recovery and daily monitoring, consider using a simple digital tool:
Check this recommended tool here →
Some readers also explore wellness supplements for general health support during recovery phases:
Discover this affordable solution today →
(Not a medical treatment.)
Final Thoughts: Know the Signs, Stay Prepared
Asthma is manageable, but only if you respect the warning signs. Strong asthma self care routines make you more aware of symptom shifts, while a clear action plan helps you respond calmly and effectively. Trust your instincts, act early, and never hesitate to seek help when breathing changes feel unusual or severe.
Your lungs rely on you to pay attention — and with the right awareness, tools, and support, you can stay safe, stable, and confident in every season.

Conclusion
Asthma may be a lifelong condition, but it does not have to limit your life. When you understand your triggers, follow a clear action plan, and build consistent habits, you gain far more control over your breathing than you might realize. Each chapter in this guide was designed to give you practical ways to strengthen your lungs, stabilize symptoms, and feel more confident every day.
Strong asthma self care is not about perfection. It’s about small, steady choices that help your airways stay calm. Whether it’s improving your home environment, managing stress, staying active, or tracking symptoms, every thoughtful step creates a healthier foundation for your lungs. And when you know when to seek medical help, you protect yourself from emergencies before they escalate.
You deserve predictable breathing, peaceful sleep, and the freedom to enjoy your days without fear of flare-ups. With the right strategies, support, and awareness, that kind of stability becomes possible. Keep building your routine, keep learning your patterns, and most importantly — keep listening to your body. Your lungs will thank you.
If you want help tracking your habits or supporting your wellness, you may find this helpful:
Check this recommended tool here →
Affiliate Disclosure
Some of the links in this article are affiliate links. This means that if you click a link and make a purchase, I may earn a small commission at no additional cost to you. These commissions help support this website and allow me to continue creating helpful, research-backed content. I only recommend products or services that I believe provide genuine value to readers.
If you’re exploring wellness options, here is one affordable solution many readers review:
Discover this affordable solution today →
Medical Disclaimer
This article is for informational and educational purposes only. It is not intended to diagnose, treat, cure, or prevent any disease. The information provided here should not replace professional medical advice, diagnosis, or treatment from a qualified healthcare provider.
Always consult your doctor before making changes to your asthma medication, treatment plan, exercise routine, or lifestyle. Never ignore medical advice or delay seeking care because of information you read online.
If you experience severe symptoms or difficulty breathing, seek emergency medical attention immediately.
Please log in to access your exclusive content.
Don’t have an account? Click the “Register” button below to sign up.










